Click for SiteMap
This is an old revision of the document!
Table of Contents
Orthopedics
Physical Therapy
must follow this guys references in detail:
https://www.painscience.com/articles/pseudo-quackery.php
METH Instead of RICE for Injuries
Lumbar
Gel Reconstruction
Hydrogels in Spinal Cord Injury Repair: A Review, Ly et al 2022
Future work on hydrogels should focus on how to modify their properties, improve their loading capacity, promote cell proliferation and differentiation, and release drugs and factors reasonably and effectively as well as explore more suitable and effective novel hydrogel scaffold materials, construct a combined treatment of hydrogel-carrying cells and drugs, and improve the microenvironment of the injured area to achieve complete repair of SCI.
11 Treatment Options for Herniated Discs, Mark Wang MD 2022 on sciatica.com
Along with a microdiscectomy, a new treatment for herniated discs involves hyaluronic acid (HA) gel and collagen gel. The HA gel re-inflates the disc, while the collagen gel seals the hole to prevent further prolapse. Ask your doctor about this treatment option with a microdiscectomy.
Based on our previous success in using NT3-chitosan to repair acute SCI in rats and monkeys, it is likely that this NT3-chitosan material, after proven safe, should be ready for clinical trials to treat subacute and chronic SCI.
Like patching a flat tire: New fix heals herniated discs, sciencedaily.com
A new two-step technique to repair herniated discs uses hyaluronic acid gel to re-inflate the disc and collagen gel to seal the hole, essentially repairing ruptured discs like you'd repair a flat tire.
Artificial Disc Replacement
Ankle
Ankle Osteoarthritis
Shoulder
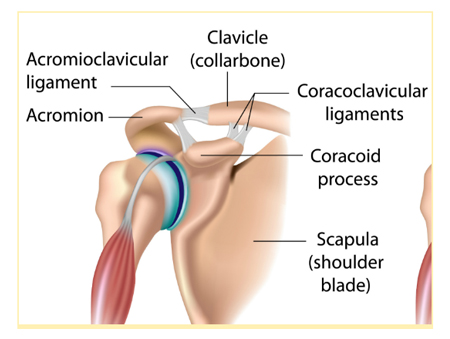
AC Joint Surgery
Shoulder acromioclavicular joint reconstruction options and outcomes
Curr Rev Musculoskelet Med. 2016 Dec; 9(4): 368–377.
Published online 2016 Sep 19. doi: 10.1007/s12178-016-9361-8
PMCID: PMC5127941, PMID: 27645218
Simon Lee1 and Asheesh Bedi
“ Adhesive capsulitis, also known as frozen shoulder, is a chronic inflammation of the shoulder capsule that causes abnormal tissue growth around the area, significantly restricting movement.
Other symptoms associated with this condition include pain and overall stiffness, often worsening at night and when it is cold. The cause of the condition is unknown, although some believe it may be linked to autoimmune complications. It occurs very rarely in individuals under the age of 40 and somewhat more frequently in those who exhibit risk factors such as:
Connective tissue disorders
Heart disease/previous stroke
Diabetes
Lung disease
Physical trauma to shoulder
Treatment for this condition varies widely from simple non-steroidal anti-inflammatory drugs (NSAIDs) and light physical therapy, to invasive surgery designed to release the excess scar tissue. The doctor may opt for manipulation under anesthesia (MUA) as a sort of middle ground to break up scar tissue without an invasive procedure. This also stimulates fluid circulation into the shoulder, which is very helpful in progressed cases of frozen shoulder. ” source
Ligament Reconstruction
Allograft versus Autografts
Allografts for Ligament Reconstruction: Where Are We Now?
Am J Orthop. 2016 November;45(7):446-452
By Frank B. Wydra MD; Philip J. York MD; Christopher R. Johnson; Lorenzo Silvestri MD
https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/ajo045110446.PDF
NSAIDS
Sports medicine physicians often treat athletes in pain with non-steroidal anti-inflammatory drugs (NSAIDs). However, there is a lack of high-quality evidence to guide NSAID use. Their adverse effects have clinical relevance, and their possible negative consequences on the long-term healing process are slowly becoming more obvious. This article provides some practical management guidelines for the use of NSAIDs, developed to help sports medicine physicians deal with frequent sports-related injuries. We do not recommend their use for muscle injuries, bone fractures (also stress fractures) or chronic tendinopathy. In all cases, if chosen, NSAID treatments should always be kept as short as possible and should take into account the specific type of injury, the level of dysfunction and pain. Non-steroidal anti-inflammatory drugs for athletes: An update, Ziltener and Fournier 2010


Discussion