Table of Contents
Orthopedics
Physical Therapy
must follow this guys references in detail:
https://www.painscience.com/articles/pseudo-quackery.php
METH Instead of RICE for Injuries
Medical Tourism
(under construction)
Medical Tourism Statistics 2024 By Landscape, Healthcare, Treatments by Trishita Deb at market.us. May be a non-biased review?
Regenerative Medicine Therapy in Malaysia: An Update, Imran et al 2022. Mentions a few countries.
Lumbar
I don't think traditional surgeries have a chance of improving a degenerative spine. Cutting away at some pieces or removing the capacity for motion at a disc doesn't sound like much of an improvement. So I focus on the topics below that might restore the spine's original structure. Supporting my view is Goobie, a neurosurgeon. See Goobie and Doobie, and make sure the playback speed is at least 1.5x. I don't think Goobie had access to these new methods. I do think living a healthy life helps, but for myself I need some extra help due to PTSD supplying a base level of anxiety.
Also interesting:
“My understanding is most people have disc degeneration and/or herniations with no symptoms of pain. There’s new research showing chronic pain is caused in part by nervous system hyper-sensitization. Most treatments that target a physical injury or damaged tissue don’t work because the pain is actually being caused by the brain, not the discs.” lifeshardandweird on Reddit
Gel Reconstruction
https://www.reddit.com/r/backpain/comments/1bibfet/my_real_time_discseel_experience
The current status and development trend of hydrogel application in spinal surgery, Qui et al 2023 Drluo2022@163.com
A total of 1099 articles pertaining to hydrogel therapy for spinal cord injury were retrieved, revealing an upward trajectory in both annual publication volume and cumulative publication volume. Biomaterials emerged as the journal with the highest number of publications and the most rapid cumulative publication growth, contributing 84 articles. Among authors, Shoichet MS stood out with the highest number of publications and citations, totaling 66 articles. The University of Toronto led in institutional contributions with 65 publications, while China dominated in country-specific publications, accounting for 374 articles. However, to foster significant academic achievements, it is imperative for diverse authors, institutions, and countries to enhance collaboration. Current research in this field concentrates on scaffold architecture, nerve growth factor, the fibrotic microenvironment, and guidance channels. Simultaneously, upcoming research directions prioritize 3D bioprinting, injectable hydrogel, inflammation, and nanoparticles within the realm of hydrogel therapy for spinal cord injuries.
From 2857 records found in MEDLINE and EMBASE databases (April 23, 2021), 49 articles were included based on our inclusion/exclusion criteria. All studies discussing the effect of hydrogels on at least one of the main pathophysiological events after TSCI, including inflammation, axon growth, remyelination, glial scar formation, cavity size, and locomotor functional recovery were included. For statistical analysis, we used mean difference with 95% confidence intervals for locomotor functional recovery. The results showed that both natural and synthetic hydrogels could reduce the inflammatory response, hinder glial scar formation, and promote axon growth and vascularization. Also, the meta-analysis of the BBB score showed that using the hydrogels can lead to locomotor functional recovery. It was found that hydrogels are more efficient when used in transection and hemisection injuries (SMD: 1.89; 95% CI: 1.26, 2.52; P < .00001) compared to other injury models. The pre-formed implanted hydrogels (SMD: 1.79; 95% CI: 1.24, 2.34; P < .00001) found to be more effective compared to injection (SMD: 1.58; 95% CI: 0.64, 2.52; P = 0.0009).
This early feasibility study showed that the hydrogel implant was safe with no persistently symptomatic SAEs (serious adverse events), and demonstrated effectiveness with significant reduction in pain and improvement in function when used to treat painful DDD (degenerative disc disease) and CLBP (chronic low back pain).
Hydrogel-based treatments for spinal cord injuries, Jia et al 2023
However, issues and challenges remain that need to be addressed by researchers. Designing hydrogels that are more compatible with the stiffness and elasticity of spinal cord tissue can help to better repair SCIs, but few researchers have worked on this to date. A particularly important feature that needs to be investigated is the swelling of the hydrogel. Hydrogel swelling may lead to compression of normal spinal cord tissues or even increase intracranial pressure, resulting in more serious complications. In addition, most previous research has focused on animal models and determining whether their findings can be applied to humans. Animal models similar to humans, such as primates, can be used. However, clinical trials in humans are required before any definitive conclusions can be drawn.
Hydrogel scaffolds in the treatment of spinal cord injury: a review, Cai et al 2023
Numerous studies to date have shown significant efficacy of combined treatment with cells, hydrogels, and active factors in animal SCI models. However, few clinical trials have been conducted to treat SCI patients with a combination of these three. The therapeutic approach of hydrogel-loaded cells and active factors still has a long way to go from animal experiments to clinical application. Firstly, the quality of the composite scaffolds needs to be ensured. The production of hydrogel scaffolds for human transplantation requires stricter manufacturing practices and quality control. Secondly, in order to achieve better efficacy, the combination of hydrogels, cells, and factors in terms of types and quantities needs to be explored.
Hydrogels in Spinal Cord Injury Repair: A Review, Ly et al 2022
Future work on hydrogels should focus on how to modify their properties, improve their loading capacity, promote cell proliferation and differentiation, and release drugs and factors reasonably and effectively as well as explore more suitable and effective novel hydrogel scaffold materials, construct a combined treatment of hydrogel-carrying cells and drugs, and improve the microenvironment of the injured area to achieve complete repair of SCI.
11 Treatment Options for Herniated Discs, Mark Wang MD 2022 on sciatica.com
Along with a microdiscectomy, a new treatment for herniated discs involves hyaluronic acid (HA) gel and collagen gel. The HA gel re-inflates the disc, while the collagen gel seals the hole to prevent further prolapse. Ask your doctor about this treatment option with a microdiscectomy.
Based on our previous success in using NT3-chitosan to repair acute SCI in rats and monkeys, it is likely that this NT3-chitosan material, after proven safe, should be ready for clinical trials to treat subacute and chronic SCI.
Engineering a biomimetic integrated scaffold for intervertebral disc replacement, Du et al 2019
Tissue engineering technology provides a promising alternative to restore physiological functionality of damaged intervertebral disc (IVD). Advanced tissue engineering strategies for IVD have increasingly focused on engineering IVD regions combined the inner nucleus pulposus (NP) and surrounding annulus fibrosus (AF) tissue. However, simulating the cellular and matrix structures and function of the complex structure of IVD is still a critical challenge. Toward this goal, this study engineered a biomimetic AF-NP composite with circumferentially oriented poly(ε-caprolactone) microfibers seeded with AF cells, with an alginate hydrogel encapsulating NP cells as a core. Fluorescent imaging and histological analysis showed that AF cells spread along the circumferentially oriented PCL microfibers and NP cells colonized in the alginate hydrogel similar to native IVD, without obvious migration and mixing between the AF and NP region. Engineered IVD implants showed progressive tissue formation over time after subcutaneous implantation in nude mice, which were indicated by deposition and organization of extracellular matrix and enhanced mechanical properties. In terms of form and function of IVD-like tissue, our engineered biomimetic AF-NP composites have potential application for IVD replacement.
Like patching a flat tire: New fix heals herniated discs, sciencedaily.com
A new two-step technique to repair herniated discs uses hyaluronic acid gel to re-inflate the disc and collagen gel to seal the hole, essentially repairing ruptured discs like you'd repair a flat tire.
Artificial Disc Nucleus
An artificial disc nucleus is designed to replace only the degenerative nucleus; most of the annulus is left intact. This device consists of a hydrogel core that can absorb fluid and expand when implanted. Partial disc replacement is also referred to as a nucleus arthroplasty. blue cross blue shield
Artificial Disc Replacement
The Blue Cross Blue Shield report gives a meager positive result ratio for ADR, though better than spinal fusion.
One study reads: “64% of ProDisc subjects and 45% of the fusion group achieved overall success (53% and 41%, respectively, by the FDA’s definitions)”.
Another study found Activel superior to ProDisc and Charité: “Freedom from a serious adverse event through five years was 64% in activL patients, 47% in control patients.”
I'd like a more fool-proof solution.
Ankle
Ankle Osteoarthritis
Shoulder
AC Joint Surgery
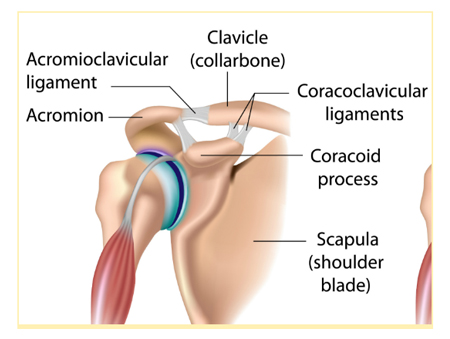
Shoulder acromioclavicular joint reconstruction options and outcomes
Curr Rev Musculoskelet Med. 2016 Dec; 9(4): 368–377.
Published online 2016 Sep 19. doi: 10.1007/s12178-016-9361-8
PMCID: PMC5127941, PMID: 27645218
Simon Lee1 and Asheesh Bedi
“ Adhesive capsulitis, also known as frozen shoulder, is a chronic inflammation of the shoulder capsule that causes abnormal tissue growth around the area, significantly restricting movement.
Other symptoms associated with this condition include pain and overall stiffness, often worsening at night and when it is cold. The cause of the condition is unknown, although some believe it may be linked to autoimmune complications. It occurs very rarely in individuals under the age of 40 and somewhat more frequently in those who exhibit risk factors such as:
Connective tissue disorders
Heart disease/previous stroke
Diabetes
Lung disease
Physical trauma to shoulder
Treatment for this condition varies widely from simple non-steroidal anti-inflammatory drugs (NSAIDs) and light physical therapy, to invasive surgery designed to release the excess scar tissue. The doctor may opt for manipulation under anesthesia (MUA) as a sort of middle ground to break up scar tissue without an invasive procedure. This also stimulates fluid circulation into the shoulder, which is very helpful in progressed cases of frozen shoulder. ” source
Ligament Reconstruction
Allograft versus Autografts
Allografts for Ligament Reconstruction: Where Are We Now?
Am J Orthop. 2016 November;45(7):446-452
By Frank B. Wydra MD; Philip J. York MD; Christopher R. Johnson; Lorenzo Silvestri MD
https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/ajo045110446.PDF
NSAIDS
Sports medicine physicians often treat athletes in pain with non-steroidal anti-inflammatory drugs (NSAIDs). However, there is a lack of high-quality evidence to guide NSAID use. Their adverse effects have clinical relevance, and their possible negative consequences on the long-term healing process are slowly becoming more obvious. This article provides some practical management guidelines for the use of NSAIDs, developed to help sports medicine physicians deal with frequent sports-related injuries. We do not recommend their use for muscle injuries, bone fractures (also stress fractures) or chronic tendinopathy. In all cases, if chosen, NSAID treatments should always be kept as short as possible and should take into account the specific type of injury, the level of dysfunction and pain. Non-steroidal anti-inflammatory drugs for athletes: An update, Ziltener and Fournier 2010